PREHAB – HOW TO PREPARE TO GET THE MOST OUT OF YOUR TREATMENT.
#1. OPTIMIZE YOUR LIFESTYLE
This can contribute up to 70% of your success as an optimal lifestyle and environment is important to the healing process. Remember, regenerative injections depend on YOUR body’s own healing response to be effective. Ways in which you can optimize your lifestyle include:
Anti-inflammatory Diet
- Include lots of colourful vegetables, berries, SMASH fish (salmon, mackerel, anchovies, sardines, herring), nuts and seeds, avocadoes.
- Balance your meals by including a healthy fat (nuts, seeds, oil, fish), protein (grass-fed and hormone-free lean meats, fish, organic tofu, chickpeas, beans, lentils), fibre (vegetables) and carbohydrate (brown rice, quinoa, sweet potato, yam)
- Cook with avocado oil, and dress salads with olive oil.
- Stay hydrated by starting your day with water and limiting caffeinated beverages to 1-2/day.
- Limit processed foods, dairy, refined sugars, fruit juices and sodas.
Daily Movement
Move daily if your body is physically able. This can mean 10-minute walks on your work breaks, going to the gym, yoga, hiking, starting your day with qi gong, swimming at the lake, dog walks, or taking your bike to work. Exercise should always leave you feeling better. If it doesn’t, try something new.
Prioritize Sleep
As Mathew Walker says, “sleep is the #1 performance enhancing drug”. It’s anabolic and the optimal time for our body to repair and refuel.
Stop or Limit Smoking and Alcohol Use
Tobacco and alcohol are toxic to our bodies, especially in high amounts, and can hinder our ability to repair. Smoking also depletes vitamin C, an essential component of healing.
Optimize Hormone Status
Hormones such as estrogen, progesterone, testosterone, cortisol, and thyroid hormones can all impact the ability to heal. Ask your naturopathic doctor to address imbalances if you are experiencing menopausal symptoms, irregular periods or PMS, low energy, insomnia, or any other symptoms you feel might be representative of hormone status.
Prioritize Mental and Emotional Well-being
Listen to your body. Even 5-minutes for yourself can greatly reduce stress. Make time for relaxation, meditation, hobbies, and/or activities that bring joy. Self-care should always decrease stress and never heighten enhance. Hence, it should never feel forced but, rather, satiating. For example, if you don’t feel like journaling, then don’t. Perhaps you are craving a round of golf or a nap instead.
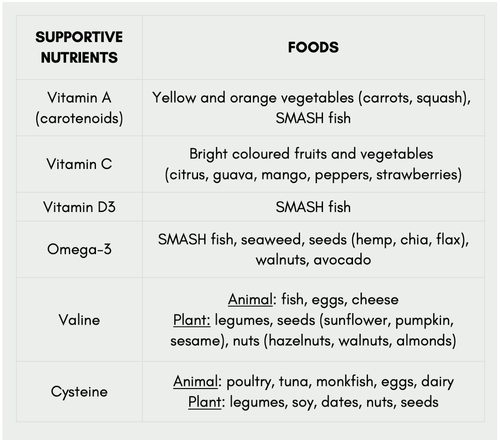
Supplementation
Consider a few key supplements such as magnesium bisglycinate (especially if taking certain anti-depressants or proton pump inhibitors, which can lower magnesium needed for repair), vitamin D, vitamin C, and fish oil. Ask your naturopathic doctor for good quality brands and optimal dosing strategies.
#2. PHYSIOTHERAPY
If you haven’t seen a physiotherapist already, book an appointment in the second week after PRP. This can help correct underlying imbalances that may have contributed to the injury. Addressing the cause is important to get for long-lasting results.
#3. SUPPLEMENTAL THERAPIES
There are a variety of therapeutic tools that can be used to enhance healing. These include:
- Massage
- Shockwave
- Ultrasound
- Laser
- Acupuncture
- Voodoo floss
- Hydrotherapy (e.g., cold plunges, Epsom salt baths, contrast hydrotherapy)
- Foam rolling
#4. EXERCISE PRIOR TO YOUR PRP TREATMENT
A 4-minute bout of high intensity exercise shortly before drawing blood (within ½ hour) can increase platelet yields in the blood. For example, it might be beneficial to bike or run to your appointment, ride a stationary bike for 4 minutes, or perform jumping jacks prior to the blood draw.
Note: Only do this if you do not have a heart condition or any other circumstances in which this could cause harm.
#5. MEDICATION EVALUATION
Prior to receiving injections, talk with the administering physician about all the current medications and supplements you’re taking to ensure they don’t interfere with the treatment and healing response. Some important medications and supplements to note include:
- Anti-inflammatories: It is generally recommended to stop anti-inflammatory medications and supplements at least 1-2 weeks (depending on strength) before and after prolotherapy as anti-inflammatories can counteract the therapeutic effect. Examples include NSAIDs (e.g., Advil/Ibuprofen, Aleve, Celebrex, Aspirin/ASA, Diclofenac/Voltaren), steroids (e.g., Prednisone, Dexamethasone, Hydrocortisone), and natural supplements (e.g., turmeric, fish oil).
- Anti-depressants, PPI’s: Don’t typically need to be discontinued but can decrease magnesium levels, thus making supplementation important.
Note: Do not stop prescribed medications without first discussing with your doctor.
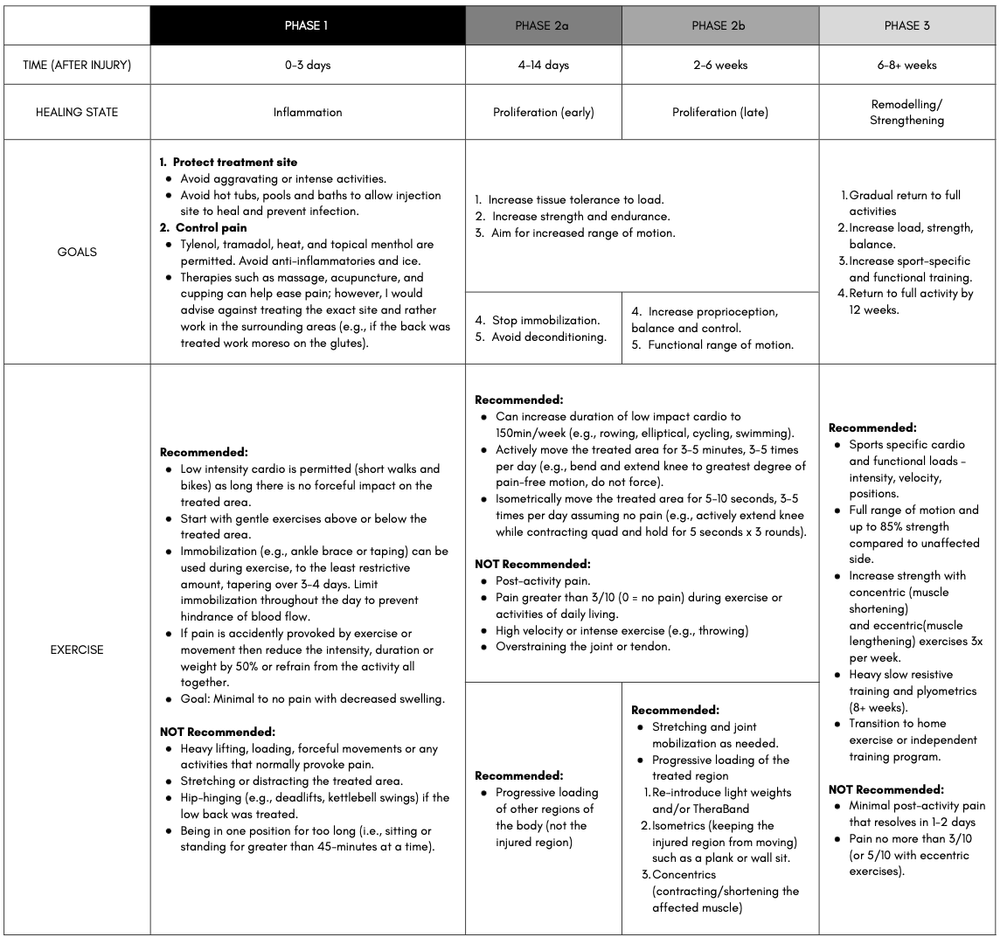
REHAB – POST PROCEDURE REHABILITATION
Overview: What to Expect
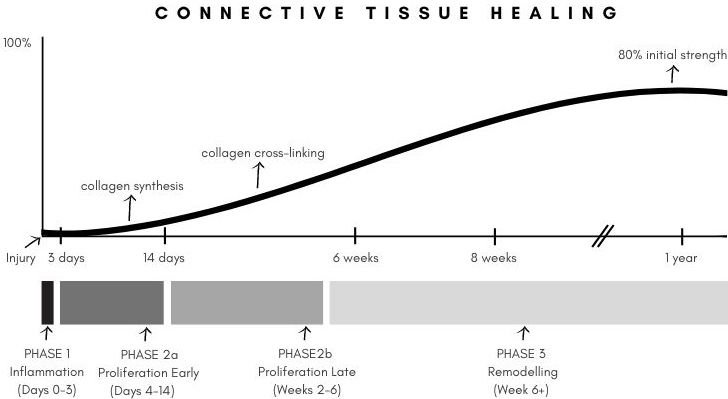
- It’s normal to experience soreness and swelling for 2-3 days after the injections. However, injections into the tendon and ligaments can sometimes be painful for 7-10 days. After this, the improvement is gradual and can take anywhere from 3 months to 2 years.
- There will be ups and downs, and adjustments will need to be made throughout the upcoming months.
CLICK HERE TO WATCH AN INFORMATIONAL VIDEO!
REFERENCES
- Abate, M., Di Carlo, L., & Salini, V. (2019). Platelet rich plasma compared to dry needling in the treatment of non-insertional achilles tendinopathy. The Physician and Sports Medicine, 47(2), 232-237. https://doi.org/10.1080/00913847.2018.1548886
- Agathocleous, M., Meacham, C,. Burgess, R. et al. (2017). Ascorbate regulates hematopoietic stem cell function and leukaemogenesis. Nature, 549, 476-481. https://doi.org/10.1038/nature23876
- Alderman, D. (2007). Prolotherapy for low back pain: A reasonable and conservative approach to MSK low back pain, disc disease, and sciatica. Retrieved from https://www.bowlermedical.org/uploads/3/9/3/5/39351519/low_back_prolo_case_studies.pdf
- Alves, R., Grimalt, R. (2018; 2017). A review of platelet-rich plasma: History, biology, mechanism of action, and classification. Skin Appendage Disorders, 4(1), 18-24. https://doi.org/10.1159/000477353
- Andia, I., Rubio-Azpeitia, E., & Maffulli, N. (2015). Platelet-rich plasma modulates the secretion of Inflammatory/Angiogenic proteins by inflamed tenocytes. Clinical Orthopaedics and Related Research, 473(5), 1624-1634. https://doi.org/10.1007/s11999-015-4179-z
- Bradley, J. P., Lawyer, T. J., Ruef, S., Towers, J. D., & Arner, J. W. (2020). Platelet-rich plasma shortens return to play in national football league players with acute hamstring injuries. Orthopaedic Journal of Sports Medicine, 8(4), 2325967120911731-2325967120911731. https://doi.org/10.1177/2325967120911731
- Brown, Hal (2015, October 29). Running injuries & rit: relief from chronic pain. Retrieved from https://ndnr.com/mens-health/running-injuries-rit-relief-from-chronic-pain/
- Cabezas-Wallscheid, N., Buettner, F., Sommerkamp, P., Klimmeck, D., Ladel, L., Thalheimer, F. B., et al (2017). Vitamin A-retinoic acid signaling regulates hematopoietic stem cell dormancy. Cell, 169(5), 807-823. https://doi.org/10.1016/j.cell.2017.04.018
- Ciftci, H., Yeni, E., Demir, M., Yagmur, I., Gümüş, K., Celik, H., Savas, M., & Gulum, M. (2013). Can the mean platelet volume be a risk factor for vasculogenic erectile dysfunction? The World Journal of Men’s Health, 31(3), 215-219. https://doi.org/10.5534/wjmh.2013.31.3.215
- Cortes, M., Chen, M., Stachura, D., Liu, S., Kwan, W., Wright, F., Vo, L., Theodore, L., Esain, V., Frost, I., Schlaeger, T., Goessling, W., Daley, G., & North, T. (2016). Developmental vitamin D availability impacts hematopoietic stem cell production. Cell Reports (Cambridge), 17(2), 458-468. https://doi.org/10.1016/j.celrep.2016.09.012
- Danieli, M. V., Pereira, H. d. R., Carneiro, Carlos Augusto de Sá, Felisbino, S. L., & Deffune, E. (2014). Treatment of osteochondral injuries with platelet gel. Clinics (São Paulo, Brazil), 69(10), 694-698. https://doi.org/10.6061/clinics/2014(10)08
- Deal, J. B., Smith, E., Heard, W., O’Brien, M. J., & Savoie, F. H. (2017). Platelet-rich plasma for primary treatment of partial ulnar collateral ligament tears: MRI correlation with results. Orthopaedic Journal of Sports Medicine, 5(11), 2325967117738238-2325967117738238. https://doi.org/10.1177/2325967117738238
- Fitzpatrick, J,. Bulsara, M. K., O’Donnel, J., & Zheng, M. H. (2019). Leucocyte-rich platelet-rich plasma treatment of gluteus medius and minimus tendinopathy: a double-blind randomization controlled trial with 2-year follow-up. The American Journal of Sports Medicine, 47(5). 1130-1137. https://doi.org/10.1177/0363546519826969
- Fonken, L. K., Aubrecht, T. G., Melendez-Fernandez, O. H., Weil, Z. M., & Nelson, R. J., (2013). Dim light and night disrupts molecular circadian rhythms and increases body weight. Journal of Biological Rhythems. 28(4), 262-271. https://doi.org/10.1177/0748730413493862
- Gasparvan, A. Y., Ayvazyan, L., Mikhailidis, D. P., & Kitas, G. D. (2001). Mean platelet volume: a link between thrombosis and inflammation? Current Phamarceutical Design, 17(1), 47-58. https://doi.org/10.2174/138161211795049804
- Haker, E., Egekvist, H., & Bjerring, P. (2000). Effect of sensory stimulation (acupuncture) on sympathetic and parasympathetic activities in healthy subjections. Journal of the Autonomic Nervous System, 79(1), 52-59. https://doi.org/10.1016/s0165-1838(99)00090-9
- Halpern, B., Chaudhury, S., Rodeo, S. A., Hayter, C., Bogner, E., Potter, H. G., & Nguyen, J. (2013). Clinical and MRI outcomes after platelet-rich plasma treatment for knee osteoarthritis. Clinical Journal of Sport Medicine, 23(3), 238-239. https://doi.org/10.1097/JSM.0b013e31827c3846
- Han, C., Na, Y., Zhu, Y., Kong, L., Eerdun, T., Yang, X., & Ren, Y. (2019). Is platelet-rich plasma an ideal biomaterial for arthroscopic rotator cuff repair? A systematic review and meta-analysis of randomized controlled trials. Journal of Orthopaedic Surgery and Research, 14(1), 183-183. https://doi.org/10.1186/s13018-019-1207-9
- Harrison, T. E., Bowler, J., Levins, T. N., Cheng, A., & Reeves, K. D. (2020). Platelet yield and yield consistency for six single-spin methods of platelet rich plasma preparation. Platelets (Edinburgh), 31(5), 661-666. 661-666. https://doi.org/10.1080/09537104.2019.1663808
- Harrison, T. E., Bowler, J., Levins, T. N., Cheng, A., & Reeves, K. D. (2020). Platelet-rich plasma centrifugation changes leukocyte ratios. Cureus (Palo Alto, CA), 13(4), e14470-e14470. https://doi.org/10.7759/cureus.14470
- Heber, S., & Volf, I. (2015). Effects of physical (in)activity on platelet function. BioMed Research International, 2015, 165078-11. https://doi.org/10.1155/2015/165078
- Heidt, T., Sager, H. B., Courties, G., Dutta, P., Iwamoto, Y., Zaltsman, A., von Zur Muhlen, C., Bode, C., Fricchione, G. L., Denninger, J., Lin, C. P., Vinegoni, C., Libby, P., Swirski, F. K., Weissleder, R., & Nahrendorf, M. (2014). Chronic variable stress activates hematopoietic stem cells. Nature Medicine, 20(7), 754-758. https://doi.org/10.1038/nm.3589
- Herdea, A., Struta, A., Derihaci, R. P., Ulici, A., Costache, A., Furtunescu, F., Toma, A., & Charkaoui, A. (2022). Efficiency of platelet-rich plasma therapy for healing sports injuries in young athletes. Experimental and Therapeutic Medicine, 23(3)https://doi.org/10.3892/etm.2022.11139
- Hicks, J. J., Li, H., Philippon, M. J., Hurwitz, S. R., Huard, J., & Hogan, M. V. (2016). Customized platelet-rich plasma for skeletal muscle injuries. Orthopaedic Journal of Sports Medicine, 4(7_suppl4), 2325967116. https://doi.org/10.1177/2325967116S00143
- Hubbard, G. P., Wolffram, S., Lovegrove, J. A., & Gibbins, J. M. (2004). Ingestion of quercetin inhibits platelet aggregation and essential components of the collagen‐stimulated platelet activation pathway in humans. Journal of Thrombosis and Haemostasis, 2(12), 2138-2145. https://doi.org/10.1111/j.1538-7836.2004.01067.x
- Iwamura, C., Bouladoux, N., Belkaid, Y., Sher, A., & Jankovic, D. (2017). Sensing of the microbiota by NOD1 in mesenchymal stromal cells regulates murine hematopoiesis. Blood, 129(2), 171–176. https://doi.org/10.1182/blood-2016-06-723742
- Johal, H., Khan, M., Yung, S. P., Dhillon, M. S., Fu, F. H., Bedi, A., & Bhandari, M. (2019). Impact of platelet-rich plasma use on pain in orthopaedic surgery: A systematic review and meta-analysis. SAGE Publications. https://doi.org/10.1177/1941738119834972
- Josefsdottir, K. S., Baldridge, M. T., Kadmon, C. S., & King, K. Y. (2017). Antibiotics impair murine hematopoiesis by depleting the intestinal microbiota. Blood, 129(6), 729–739. https://doi.org/10.1182/blood-2016-03-708594
- Joshi Jubert, N., Rodríguez, L., Reverté-Vinaixa, M. M., & Navarro, A. (2017). Platelet-rich plasma injections for advanced knee osteoarthritis: A prospective, randomized, double-blinded clinical trial. Orthopaedic Journal of Sports Medicine, 5(2), 2325967116689386-2325967116689386. https://doi.org/10.1177/2325967116689386
- Kaminski, R., Kulinski, K., Kozar-Kaminska, K., Wielgus, M., Langner, M., Wasko, M. K., Kowalczewski, J., & Pomianowski, S. (2018). A prospective, randomized, double-blind, parallel-group, placebo-controlled study evaluating meniscal healing, clinical outcomes, and safety in patients undergoing meniscal repair of unstable, complete vertical meniscal tears (bucket handle) augmented with platelet-rich plasma. BioMed Research International, 2018, 9315815-9. https://doi.org/10.1155/2018/9315815
- Kraeutler, M. J., Houck, D. A., Garabekyan, T., Miller, S. L., Dragoo, J. L., & Mei-Dan, O. (2021). Comparing intra-articular injections of leukocyte-poor platelet-rich plasma versus Low–Molecular weight hyaluronic acid for the treatment of symptomatic osteoarthritis of the hip: A double-blind, randomized pilot study. Orthopaedic Journal of Sports Medicine, 9(1), 2325967120969210-2325967120969210. https://doi.org/10.1177/2325967120969210
- Li, Y., Zhu, S., Zhang, Y., Liu, T., Su, L., Zhang, Q., & Luo, Y. (2018). High fat diet-induced obesity exacerbates hematopoiesis deficiency and cytopenia caused by 5-fluorouracil via peroxisome proliferator-activated receptor γ. Experimental hematology, 60, 30–39.e1. https://doi.org/10.1016/j.exphem.2017.12.013
- Luo, Y., Chen, G., Hannemann, N., Ipseiz, N., Krönke, G., Bäuerle, T., Munos, L., Wirtz, S., Schett, G., & Bozec, A. (2015). Microbiota from obese mice regulate hematopoietic stem cell differentiation by altering the bone niche. Cell Metabolism, 22(5), 886-894. https://doi.org/10.1016/j.cmet.2015.08.020
- Marshall, D. A., Liu, X., Barnabe, C., Yee, K., Faris, P. D., Barber, C., Mosher, D., Noseworthy, T., Werle, J., & Lix, L. (2019). Existing comorbidities in people with osteoarthritis: A retrospective analysis of a population-based cohort in alberta, canada. BMJ Open, 9(11), e033334-e033334. https://doi.org/10.1136/bmjopen-2019-033334
- Mascarenhas, R., Saltzman, B. M., Fortier, L. A., & Cole, B. J. (2015). Role of platelet-rich plasma in articular cartilage injury and disease. The Journal of Knee Surgery, 28(1), 003-010. https://doi.org/10.1055/s-0034-1384672
- Mills, F. B., Misra, A. K., Goyeneche, N., Hackel, J. G., Andrews, J. R., & Joyner, P. W. (2021). Return to play after platelet-rich plasma injection for elbow UCL injury: Outcomes based on injury severity. Orthopaedic Journal of Sports Medicine, 9(3), 2325967121991135-2325967121991135. https://doi.org/10.1177/2325967121991135
- Murphy, K. J., Chronopoulos, A. K., Singh, I., Francis, M. A., Moriarty, H., Pike, M. J., Turner, A. H., Mann, N. J., & Sinclair, A. J. (2003). Dietary flavanols and procyanidin oligomers from cocoa (theobroma cacao) inhibit platelet function. The American Journal of Clinical Nutrition, 77(6), 1466-1473. https://doi.org/10.1093/ajcn/77.6.1466
- Murphy, E. A., Davis, J. M., Carmichael, M. D., Gangemi, J. D., Ghaffar, A., & Mayer, E. P. (2008). Exercise stress increases susceptibility to influenza infection. Brain, Behavior, And Immunity, 22(8), 1152–1155. https://doi.org/10.1016/j.bbi.2008.06.004
- Nahrendorf, M., & Swirski, F. K. (2015). Lifestyle effects on hematopoiesis and atherosclerosis. Circulation Research, 116(5), 884-894. https://doi.org/10.1161/CIRCRESAHA.116.303550
- Oliveira, D. C., Nogueira-Pedro, A., Santos, E. W., Hastreiter, A., Silva, G. B., Borelli, P., & Fock, R. A. (2018). A review of select minerals influencing the haematopoietic process. Nutrition Research Reviews, 31(2), 267–280. https://doi.org/10.1017/S0954422418000112
- Ozdemir, O., Soylu, M., Alyan, O., Geyik, B., Demir, A. D., Aras, D., Cihan, G., Cagirci, G., Kacmaz, F., Balbay, Y., Sasmaz, H., & Korkmaz, S. (2004). Association between mean platelet volume and autonomic nervous system functions: Increased mean platelet volume reflects sympathetic overactivity. Experimental and Clinical Cardiology, 9(4), 243-247.
- Pan, P., Wang, J., Tsai, C., & Kuo, H. (2022). Identification of early response to hypertonic dextrose prolotherapy markers in knee osteoarthritis patients by an inflammation-related cytokine array. Journal of the Chinese Medical Association, 85(4), 525-531. https://doi.org/10.1097/JCMA.0000000000000693
- Park, P. Y. S., Cai, C., Bawa, P., & Kumaravel, M. (2018;2019;). Platelet-rich plasma vs. steroid injections for hamstring injury—is there really a choice? Skeletal Radiology, 48(4), 577-582. https://doi.org/10.1007/s00256-018-3063-9
- Pauly, S., Klatte-Schulz, F., Stahnke, K., Scheibel, M., & Wildemann, B. (2018). The effect of autologous platelet rich plasma on tenocytes of the human rotator cuff. BMC Musculoskeletal Disorders, 19(1), 422-422. https://doi.org/10.1186/s12891-018-2339-5
- Prodromos, C. C., Finkle, S., Prodromos, A., Chen, J. L., Schwartz, A., & Wathen, L. (2021). Treatment of rotator cuff tears with platelet rich plasma: A prospective study with 2 year follow‐up. BMC Musculoskeletal Disorders, 22(1), 1-499. https://doi.org/10.1186/s12891-021-04288-4
- Ranjith, M. P., DivyaRaj, R., Mathew, D., George, B., & Krishnan, M. N. (2016). Mean platelet volume and cardiovascular outcomes in acute myocardial infarction. Heart Asia, 8(1), 16-20. https://doi.org/10.1136/heartasia-2015-010696
- Rosenwinkel, E. T., Bloomfield, D. M., Arwady, M. A., & Goldsmith, R. L. (2001). Exercise and autonomic function in health and cardiovascular disease. Cardiology Clinics, 19(3), 369–387. https://doi.org/10.1016/s0733-8651(05)70223-x
- Ruf J. C. (2004). Alcohol, wine and platelet function. Biological Research, 37(2), 209–215. https://doi.org/10.4067/s0716-97602004000200006
- Shahid, M., & Kundra, R. (2017). Platelet-rich plasma (PRP) for knee disorders. EFORT Open Reviews, 2(1), 28-34. https://doi.org/10.1302/2058-5241.2.160004
- Singer, K., DelProposto, J., Lee Morris, D., Zamarron, B., Mergian, T., Maley, N., Cho, K. W., Geletka, L., Subbaiah, P., Muir, L., Martinez-Santibanez, G., & Nien-Kai Lumeng, C. (2014). Diet-induced obesity promotes myelopoiesis in hematopoietic stem cells. Molecular Metabolism (Germany), 3(6), 664-675. https://doi.org/10.1016/j.molmet.2014.06.005
- Studzinski, G. P., Harrison, J. S., Wang, X., Sarkar, S., Kalia, V., & Danilenko, M. (2015). Vitamin D control of hematopoietic cell differentiation and leukemia: V ITAMIN D C ONTROL. Journal of Cellular Biochemistry, 116(8), 1500-1512. https://doi.org/10.1002/jcb.25104
- Swain, S., Sarmanova, A., Coupland, C., Doherty, M., & Zhang, W. (2020;2019;). Comorbidities in osteoarthritis: A systematic review and Meta‐Analysis of observational studies. Arthritis Care & Research (2010), 72(7), 991-1000. https://doi.org/10.1002/acr.24008
- Taya, Y., Ota, Y., Wilkinson, A. C., Kanazawa, A., Watarai, H., Kasai, M., Nakauchi, H., & Yamazaki, S. (2016). Depleting dietary valine permits nonmyeloablative mouse hematopoietic stem cell transplantation. Science (New York, N.Y.), 354(6316), 1152–1155.
- Thepsoparn, M., Thanphraisan, P., Tanpowpong, T., & Itthipanichpong, T. (2021). Comparison of a platelet-rich plasma injection and a conventional steroid injection for pain relief and functional improvement of partial supraspinatus tears. Orthopaedic Journal of Sports Medicine, 9(9), 23259671211024937-23259671211024937. https://doi.org/10.1177/23259671211024937
- Tischer, T., Bode, G., Buhs, M., Marquass, B., Nehrer, S., Vogt, S., Zinser, W., Angele, P., Spahn, G., Welsch, G. H., Niemeyer, P., & Madry, H. (2020). Platelet-rich plasma (PRP) as therapy for cartilage, tendon and muscle damage – german working group position statement. Journal of Experimental Orthopaedics, 7(1), 64-64. https://doi.org/10.1186/s40634-020-00282-2
- Trompette, A., Gollwitzer, E. S., Yadava, K., Sichelstiel, A. K., Sprenger, N., Ngom-Bru, C., Blanchard, C., Junt, T., Nicod, L. P., Harris, N. L., & Marsland, B. J. (2014). Gut microbiota metabolism of dietary fiber influences allergic airway disease and hematopoiesis. Nature Medicine, 20(2), 159-166. https://doi.org/10.1038/nm.3444
- Uzun, H., Bitik, O., Uzun, Ö., Ersoy, U. S., & Aktaş, E. (2017). Platelet-rich plasma versus corticosteroid injections for carpal tunnel syndrome. Journal of Plastic Surgery and Hand Surgery, 51(5), 301-305. https://doi.org/10.1080/2000656X.2016.1260025
- Valacchi, G., & Bocci, V. (1999). Studies on the biological effects of ozone: 10. release of factors from ozonated human platelets. Mediators of Inflammation, 1999(4), 205-209. https://doi.org/10.1080/09629359990360
- van den Berg, S. M., Seijkens, T. T., Kusters, P. J., Beckers, L., den Toom, M., Smeets, E., Levels, J., de Winther, M. P., & Lutgens, E. (2016). Diet-induced obesity in mice diminishes hematopoietic stem and progenitor cells in the bone marrow. FASEB Journal : Official Publication Of The Federation Of American Societies For Experimental Biology, 30(5), 1779–1788. https://doi.org/10.1096/fj.201500175
- Xia, S., Li, X., Cheng, L., Han, M., Zhang, M., Shao, Q., Xu, H., & Qi, L. (2015). Fish Oil–Rich diet promotes hematopoiesis and alters hematopoietic niche. Endocrinology (Philadelphia), 156(8), 2821-2830. https://doi.org/10.1210/en.2015-1258
- Yoshida, M., & Marumo, K. (2019;2017;). An autologous leukocyte-reduced platelet-rich plasma therapy for chronic injury of the medial collateral ligament in the knee: A report of 3 successful cases. Clinical Journal of Sport Medicine, 29(1), e4-e6. https://doi.org/10.1097/JSM.0000000000000515
- Yu, T., Pang, J. S., Lin, L., Cheng, J., Liu, S., & Tsai, W. (2021). Platelet-rich plasma releasate promotes early healing in tendon after acute injury. Orthopaedic Journal of Sports Medicine, 9(4), 2325967121990377-2325967121990377. https://doi.org/10.1177/2325967121990377
- Zhang, J., Li, F., Augi, T., Williamson, K. M., Onishi, K., Hogan, M. V., Neal, M. D., & Wang, J. H. -. (2021). Platelet HMGB1 in platelet-rich plasma (PRP) promotes tendon wound healing. PloS One, 16(9), e0251166-e0251166. https://doi.org/10.1371/journal.pone.0251166